

In childhood absence epilepsy, in which typical absence seizures are the only type of seizures affecting the child, seizures generally cease spontaneously by 12 years of age or sooner.
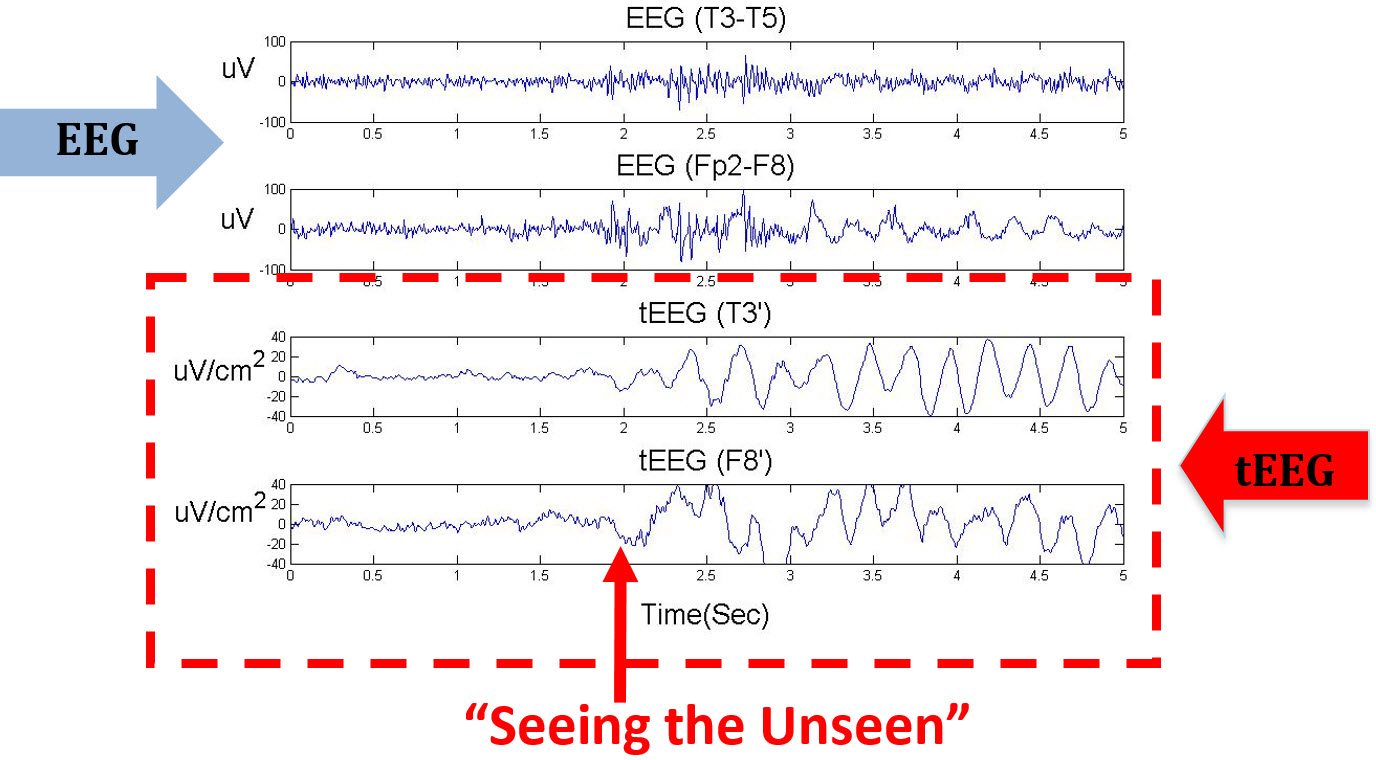
Typical absence seizures should not be confused with atypical absence seizures, which differ markedly in EEG findings and ictal behavior, and are usually present with other seizure types in a child with a background of learning disability and severe epilepsy. However, the abrupt ending of typical absence seizures, without a postictal phase, is the most useful clinical feature in distinguishing the two types. Typical absence seizures are often confused with complex partial seizures, especially in cases of prolonged seizure with automatisms. Typical absence seizures display a characteristic EEG showing regular symmetrical generalized spike and wave complexes with a frequency of 3 Hz, and usually occur in children with normal development and intelligence. Interventions for atypical absence seizures or for absence seizures secondary to structural lesions are not included in this review. atypical seizures is important, as the natural history and response to treatment vary between the two groups. On the other hand, a patient with known epilepsy could have an EEG without spikes.Absence seizures are sudden, frequent episodes of unconsciousness lasting a few seconds, and they are often accompanied by simple automatisms or clonic, atonic, or autonomic components. Therefore, an “abnormal EEG” itself does not confirm the diagnosis of epilepsy. Important: not all patients with spikes on the EEG have epilepsy (about 2% of the population without epilepsy could show spikes, and will never develop seizures or epilepsy). The spike is a “marker” of epilepsy most of the time, but does not necessarily indicate that the patient is having a seizure at that particular time. In patients with epilepsy, some electrodes (partial epilepsy) or all (generalized) epilepsy show an excess of electrical activity which is called a “spike”. Interpretation of results: In a patient without epilepsy, all the electrodes show balanced activity. exposure to flashing lights) and sleep deprivation are used to bring on epilepsy activity. On some occasions, provocative measures such as hyperventilation, photic stimulation (i.e. It usually lasts between 20 to 60 minutes. A routine EEG could be done during an awake, drowsy and/or sleep state. Different parts of the brain are being assessed since these electrodes are positioned across the scalp. This EEG machine produces graphs with waves representing the electrical activity of the brain. Technical aspects: During an EEG many electrodes are placed on the scalp to detect the electrical activity going on in the brain this is then transmitted to a machine.

EEG is an abbreviation used for electroencephalogram (a test that measures the electrical activity in the brain)


 0 kommentar(er)
0 kommentar(er)
